Does Blue Cross Blue Shield Cover Dental Implants or Just Part of the Cost?
February 6, 2026

Back to Blog
February 6, 2026

Back to Blog

Most Blue Cross Blue Shield dental plans cap annual benefits at $1,000–$2,000, but major procedures like implants, crowns, and abutments often cost $10,000–$15,000 or more, meaning patients exhaust their coverage quickly and pay most of the expense out of pocket (Medicare plans face similar limits).
With a single implant running $3,000–$6,000 and that cap covering all dental care, not just implants, routine cleanings, and part of the surgery, can use up your allowance before restoration even begins. For an All-on-4, that means paying possibly $15,000–$30,000+ out of pocket.
Implant decisions rarely go wrong because of the dentistry. They go wrong when the financial picture is unclear, claims get processed incorrectly, or patients mistake "covered" for "paid for."
Before you commit, understand these three basics so you're comparing real out-of-pocket numbers, not assumptions or vague "coverage" promises.
Blue Cross Blue Shield is an association of 33 independent companies. That means implant benefits vary widely by plan, state, and employer.
Your coworker with Anthem Blue Cross Blue Shield (Elevance Health) might have completely different coverage than you do with Blue Cross Blue Shield of Texas, Florida Blue, Independence Blue Cross, or Blue Shield of California. Start by identifying your exact plan: Is it a PPO or an HMO? Employer-sponsored or marketplace? FEP BlueDental? Then figure out whether your claim goes through dental benefits, medical benefits, or both.
An implant isn't billed as one charge. It's submitted as several parts: imaging, surgical placement of the post, possible bone grafting, and the final tooth (abutment and crown).
Insurance reviews each part separately, so approval for one part doesn't carry over to the others. What people call "implant coverage" is really a collection of separate decisions about what they'll pay.
In practice, if insurance contributes at all, it tends to pay more toward the surgical portion than the restoration. On top of that, most dental plans have an annual maximum (often $1,000–$1,500) that caps the plan's total annual payment. That limit often runs out before the final tooth is completed, which is why many patients face a large out-of-pocket balance even when something is technically "covered."
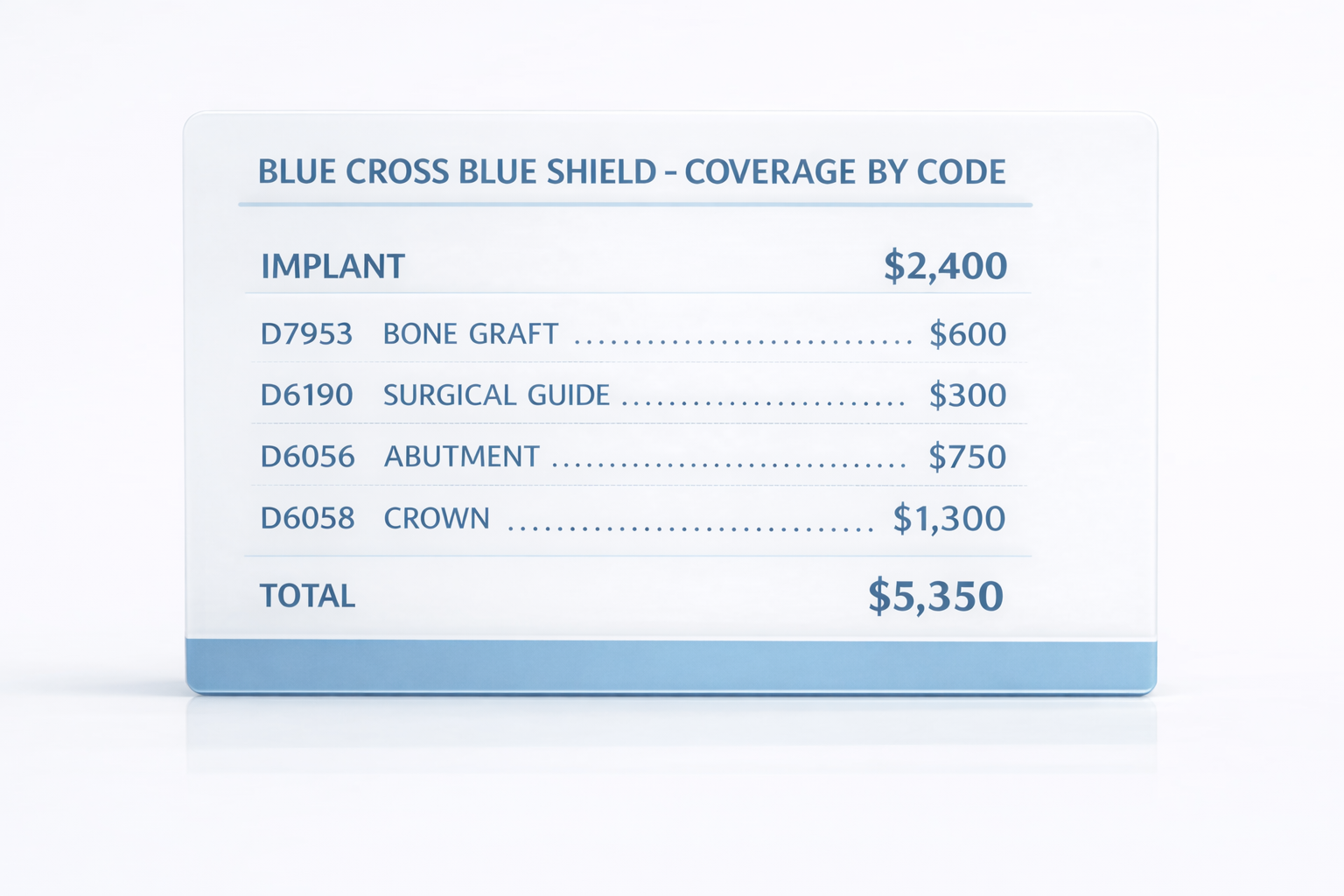
What clinics or insurers say on the phone isn't binding. The only reliable way to know what's actually covered is to check your treatment against specific billing codes:
With that paperwork in hand, you can calculate your real out-of-pocket cost and compare it directly against a bundled private quote that clearly spells out what's included, what's not, warranty terms, and aftercare.

Implant treatment is broken into multiple parts, and BCBS looks at each one under different rules. As a result, coverage often seems inconsistent across plans and even within the same treatment.
The table below shows how this typically plays out and what you should verify before relying on any estimate.
Implant coverage is one of the easiest areas for miscommunication because everything depends on codes, documentation, and timing. That's why we created the COVER framework: to give you a clear, step-by-step way to verify benefits, line up your documentation, and make decisions based on real numbers rather than guesses.
Confirm coverage for each part separately:
Common add-ons:
What to request first:
Important: If your plan uses an "alternate benefit," Blue Cross Blue Shield might pay as if you chose a bridge or denture, even if you receive an implant. That can be the difference between "covered" and "still expensive," so ask about it directly, and get the answer in writing.
To calculate what you'll actually spend, consider:
Make the comparison fair by placing your confirmed insurance costs next to a bundled clinic quote covering the same scope of work, including surgery, abutment, crown, imaging, and grafting, if clinically needed.
If the difference in your out-of-pocket cost is close to the bundled price difference, the decision usually comes down to predictability, warranty coverage, and aftercare support, not just the headline price.
Many implant billing problems happen because people skip the one step that prevents denials: getting written confirmation before treatment begins.
Use this script when you call BCBS:
If you're denied, move quickly and build a clean evidence package. Denials often come down to missing steps, missing documentation, or claims processed under the wrong benefit category.
Build your appeals folder with:
If your coverage is limited, or if the approval timeline feels uncertain, it makes sense to compare other options side by side:
What matters most when evaluating bundles isn't just price, but warranty terms (what's covered, for how long), who handles repairs once you're home, and whether you can get local follow-up if an adjustment is needed.

To make a fair comparison, focus on what you will actually pay out of pocket. Add every expected cost, including clinic fees, the implant, abutment, crown, lab work, imaging, grafting, anesthesia or sedation, temporaries, follow-up visits, and potential repairs.
If you're traveling for care, also include flights, lodging, local transportation, and time off work.
The table below breaks down what you'll typically pay out of pocket with BCBS versus what's usually included in a bundled clinic price, and how to verify each line item before you commit.
Let's say your predetermination shows that your insurance will pay part of the surgical placement, while the abutment and crown are excluded or reimbursed at a much lower rate. At the same time, part of your annual maximum has already been used earlier in the year. The result is that more of the final cost shifts back to you than you expected.
To make this concrete, write down exactly what your insurance confirmed in writing.
Check all that apply and write the billing codes shown on your plan:
For each code, ask: allowed amount, what they pay, what you pay.
Also capture:
Add only what you pay, not what insurance pays.
If travel is required:
Set aside a buffer for adjustments, repairs, or unexpected follow-ups over the next 6–24 months.
Create one folder on your phone or computer and save:
Name files with dates so nothing gets lost later.
Bottom Line: Write things down. Keep them organized. Compare real numbers instead of guesses. That's how you stay in control, rather than letting the system surprise you later.

Mexico is a popular destination for many U.S. patients because getting there and receiving treatment is simple. Flights are short, schedules are easy to line up, and recovery stays are easy to plan.
Most patients take a short flight, stay several days for surgery and early recovery, and return home with the implant placed and a clear plan for the next phase of treatment. There's no long travel, no unfamiliar systems to figure out, and no complicated coordination.
Even after flights and lodging, total costs often land 50–70% below typical U.S. out-of-pocket pricing. You get a written, itemized quote upfront that shows exactly what's included. There are no predeterminations, no approval delays, and no post-treatment denials. Costs stay predictable, and decisions stay grounded in real numbers.
The right location depends on where you live, how much time you can take off, and how much flexibility you want for travel and recovery.
Some patients want the shortest possible trip. Others prefer a more comfortable recovery setting or easier access to specialists. There's no single "best" location. Only what fits your schedule, budget, and case.

If you live in the Southwest or want to keep travel as short as possible, border clinics can be a practical option. Travel time is minimal, and logistics are straightforward.
Best fit if you want the shortest travel time and don't need resort-style accommodations.

If you can take a few extra days and want a more comfortable recovery environment, Mexico's coastal cities offer direct flights from most major U.S. hubs and well-established medical tourism infrastructure.
Best fit if comfort during recovery matters and you're comfortable staying a few days locally.

For complex cases or patients who prefer a large urban medical environment, major cities offer deeper specialist access and more scheduling flexibility.
Best fit if your case is complex or you want access to a broader specialist network.
Most implant treatments require two trips. The first visit covers implant placement and any extractions or grafting. After a healing period of roughly three to six months, the second visit completes the final crown, bridge, or full-arch restoration.
Plan two to four days onsite for a straightforward implant visit, and longer for full-arch cases that require multiple fittings and bite adjustments. Always build in at least one buffer day before flying home to allow for swelling, medication adjustments, or an unexpected follow-up check.
Compared to navigating insurance approvals, the clinical timeline is often similar, but there's less paperwork. There's no waiting weeks for predeterminations, no mid-treatment denials, and no uncertainty about what will be paid after the fact.
Once the quote is confirmed, you schedule and move forward with clear expectations.
Focus on the full path, not just the initial price. Cost, timeline, follow-up care, and warranty protection matter more than any single line item.

When insurance coverage is limited, or you want a clearer all-in number, considering cross-border dental care in Mexico can make sense, as bundled pricing often reduces billing surprises. The opportunity is real, and popular destinations like Los Algodones are considered safe for dental tourism, but so are the risks if clinics, pricing, and aftercare aren't properly vetted.
Globalcare is built for patients who want structure, transparency, and clear documentation before committing.
What Globalcare does differently:
This tends to fit best if:
Globalcare supports treatment in: Cancun, Los Cabos, Los Algodones, Puerto Vallarta, Playa del Carmen, Guadalajara, Mexico City, Queretaro, Monterrey, Ciudad Juarez, and Merida. The best location depends on your schedule, treatment complexity, comfort level, and budget.
In most BCBS dental plans, the implant crown and abutment are limited or excluded unless you have a higher-tier plan or a specific implant rider. Even when the surgical placement is partially covered, the restorative phase is usually paid largely out of pocket.
Always confirm crown coverage by billing code, for example: D6065 for an implant-supported porcelain or ceramic crown, and request written confirmation whenever possible. What you're told on the phone isn't binding and often leads to misunderstandings once claims are submitted.
Most implant claim denials happen for paperwork or process reasons, not because the treatment itself was inappropriate:
Nearly all of these issues can be avoided by confirming coverage by code in advance and keeping written confirmation.
Aftercare should be planned before you travel, not figured out after you're home. Look for written terms that clearly spell out:
If you don't have this in writing, with current contact info and a clear plan for what happens if something needs fixing, assume you'll be handling follow-up care back home and paying for it yourself. If something does go wrong, Mexico has official channels for filing dental complaints, but working with a vetted clinic network such as Globalcare lowers the odds you'll ever need them.
BCBS implant coverage varies widely by plan and is rarely all-in. The most reliable way to reduce surprise costs is to follow a simple discipline:
When each step is documented in advance, financial risk drops sharply.
If you've confirmed your codes and your out-of-pocket cost is still high, the next step is an apples-to-apples comparison of reputable clinics and complete treatment plans.
On Globalcare, clinics are vetted before joining the network. You can:
This shortens the distance between insurance uncertainty and a concrete, documented decision.
Editorial note: This article is for general education and does not provide individualized insurance, medical, or legal advice. Coverage and eligibility depend on your specific BCBS or FEP plan, clinical documentation, and compliance with plan requirements (such as waiting periods, predetermination, and preauthorization).
While we strive for accuracy, this content may contain errors, outdated information, or unintentional inconsistencies. Always verify details directly with BCBS, your plan administrator, and your treating clinician before making decisions about your care.
Get in touch to get started!
Our team of experts will ensure your all-on-4 dental implants journey is safe and easy. We're dedicated to guiding you to your new smile every step of the way!
ConnectConcierge Services

Trusted Dentists

Safe Locations

Concierge Services

Trusted Dentists

Safe Locations

Disclaimer: Dental Cost Estimation Calculator
This Dental Cost Estimation Calculator is designed to provide users with estimates of potential savings when seeking dental treatments abroad compared to the cost of similar procedures in the United States. However, please be aware of the following important information before using this tool:
1. Estimations Based on Publicly Available Data:
The estimates provided in this calculator are derived from publicly available data sources, including average procedure costs, exchange rates, and other relevant information. These figures may not reflect the exact costs of your specific treatment or location. Estimations include non-dynamic assumptions for travel and lodging costs that may not reflect the actual costs at the time of your research.
2. Quantitative Model Assumptions:
The calculations are based on assumptions and data inputs that may not account for all factors influencing dental treatment costs. Variations in individual treatment needs, dentist fees, and other variables can significantly affect the final expenses.
3. No Substitute for Professional Advice:
This tool is not a substitute for professional dental advice. Before making any decisions about your dental treatment, it is crucial to consult with a qualified dental professional who can provide you with a personalized assessment of your needs and potential costs.
4. Currency Exchange Rates:
Estimates involving foreign treatment costs rely on currency exchange rates, which can fluctuate. The rates used in this calculator may not accurately represent the current market rates at the time of your treatment.
5. Geographic and Facility Variations:
Dental costs can vary significantly based on geographic location, dental facility, and the complexity of the procedure. The estimates provided are general in nature and may not reflect the specific conditions in your chosen destination or dental clinic.
6. Non-Inclusive Costs:
This calculator may not account for additional expenses such as per diem costs in destination or unforeseen complications during or after the procedure. These costs can substantially impact your overall expenses.
7. Liability Waiver:
By using this calculator, you acknowledge that the estimates provided are for informational purposes only, and Globalcare Network Inc or any of its representatives bear no responsibility for the accuracy of the estimates or any decisions made based on them.
8. Independent Research Recommended:
It is strongly recommended that you conduct independent research, obtain quotes from dental professionals, and consider all relevant factors when making decisions about dental treatment abroad.
In summary, while this Dental Cost Estimation Calculator aims to provide helpful information, it should not be the sole basis for your decision-making process. Your individual circumstances and dental needs may differ, and it is essential to seek professional advice and conduct thorough research before pursuing dental treatment abroad